Cornea Transplantation
The cornea is the clear anterior lining of the eye, which together with the lens helps to focus light on the retina. It consists of layers of cells, which work together to protect the eye and ensure clear vision.

The cornea consists of 5 layers:
- The epithelium, which is the outer protective layer ("the skin") of the cornea.
- Bowman’s membrane
- The stroma, which is the thickest layer of the cornea. It consists of water, collagen fibers and other connective tissue, which strengthens the cornea and makes it flexible and clear.
- Descemet membrane
- The endothelium, which is the inner layer of the cornea. It consists of cells that act as pumps and remove any excess water from the stroma, thus contributing to its clarity.
Good eyesight requires a clear, smooth and healthy cornea. Corneal scars, haze and edema (swelling) do not allow for proper focusing of the incoming light, thus the vision becomes blurred or cloudy. In such cases, corneal transplantation (or keratoplasty) is recommended, i.e. replacement of the diseased cornea by a clear healthy corneal graft.
Corneal donors are those who choose to donate their corneas after death for the benefit of fellow human beings who need a corneal transplant to regain their eyesight. The donor is carefully screened for many infections and diseases, including hepatitis, syphilis and HIV/AIDS. All donor corneas used by Dr. Palioura are carefully screened for suitability by Eye Banks in the United States of America, whose operation is constantly monitored by regulatory agencies.
There are different types of corneal transplants. In some cases only the anterior and middle layers of the cornea are replaced (e.g. Deep Anterior Lamellar Keratoplasty or DALK), while in other cases only the inner layer of the cornea is replaced (e.g. Descemet Stripping Automated Endothelial Keratoplasty or DSAEK, Descemet Membrane Endothelial Keratoplasty or DMEK). Sometimes, the entire cornea needs to be replaced (penetrating keratoplasty).
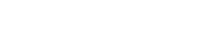
Schnyder Corneal Dystrophy
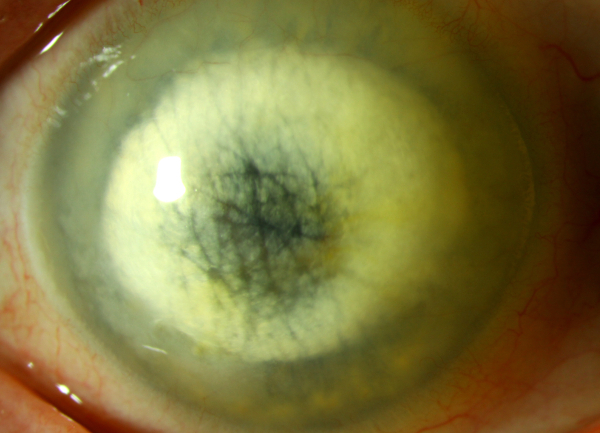
Corneal Opacification due to Chronic Edema after Cataract Surgery
Common causes that lead to corneal transplantation are:
- Keratoconus, i.e. the cornea is cone-shaped and not dome-shaped.
- Corneal stromal dystrophies (e.g. Avellino, Schnyder).
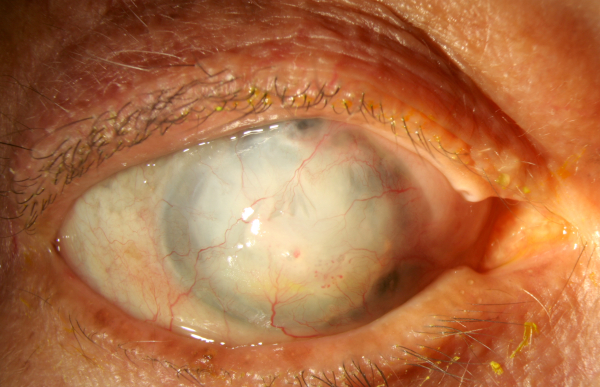
- Corneal edema due to Fuchs endothelial dystrophy or bullous keratopathy after cataract, glaucoma or vitrectomy surgery.
- Infections or injuries that cause significant corneal stromal scarring.
- Previous eye surgery that resulted in corneal dysfunction or injury.
Full-Thickness Corneal Transplantation or Penetrating Keratoplasty (PKP)
The entire cornea may need to be replaced if both the outer and inner layers are damaged. This is called penetrating keratoplasty or full-thickness corneal transplantation. The patient's cornea is removed and replaced with a healthy donor cornea.
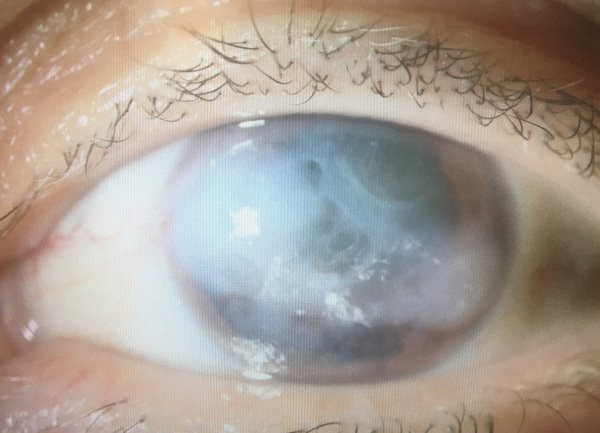
Corneal Opacification after Severe Fungal Keratitis
The most common indications for penetrating keratoplasty are corneal scars (e.g. after a corneal ulcer or after trauma), corneal dystrophies, keratoconus, chronic corneal edema (bullous keratopathy) that has resulted in corneal scarring, and a repeat transplant (that is, when the first transplant was full thickness and it has been rejected or has failed). Moreover, in cases of corneal ulcers that do not respond to medical therapy, therapeutic penetrating keratoplasty may need to be performed to clear the infection.
The most serious complication during corneal transplantation surgery is suprachoroidal hemorrhage, which can lead to total vision loss. Post-operatively, glaucoma is quite common after a full-thickness corneal transplant, as is astigmatism, which usually requires a rigid gas permeable contact lens to manage. Rarely, there may be a suture-related infection, which is treated with topical antibiotic eye drops.
Prognosis: Penetrating keratoplasty has a longer recovery period than other corneal transplants. Full visual recovery after penetrating keratoplasty can take up to a year or more. Adverse prognostic signs for the success of a full-thickness corneal transplant over time are the presence of new vessels (neovascularization) in the corneal stroma, absence of corneal sensation, and severe dry eye.
There is also a higher risk of graft rejection than in other types of corneal transplants. Rejection occurs when the recipient’s immune system attacks the donor's corneal tissue. Risk factors for full-thickness corneal transplant rejection include the presence of neovascularization, postoperative corneal infection / ulceration, large-sized grafts, and graft-to-iris (iridocorneal) adhesions.
Partial Thickness Corneal Transplantation or Deep Anterior Lamellar Keratoplasty (DALK)
Sometimes the anterior and middle layers (the stroma) of the cornea are damaged, while the inner layer (the endothelium) remains healthy. In this case, only the anterior and middle layers are removed, while the endothelium is left in place. This type of transplant is called partial-thickness corneal transplantation, anterior lamellar keratoplasty, or DALK (Deep Anterior Lamellar Keratoplasty) and is commonly used to treat advanced keratoconus and less commonly to treat certain corneal dystrophies (e.g. Avellino corneal stromal dystrophy).

Advanced Keratoconus
Avellino-type Corneal Stromal Dystrophy
The advantages of anterior lamellar keratoplasty over penetrating keratoplasty are the lack of risk for suprachoroidal hemorrhage during the operation and the lower risk of rejection of the new corneal tissue. However, the surgery itself is technically more challenging, and postoperatively clouding (haze) at the interface between the graft and the corneal endothelium may develop and result in sub-optimal quality of vision. As with penetrating keratoplasty, there can be significant astigmatism from the sutures which usually requires a rigid gas permeable contact lens to manage. Here too, a suture-related infection may develop and it can be treated with topical medications.
Prognosis: In general, healing time after anterior lamellar keratoplasty is shorter than after penetrating keratoplasty. Adverse prognostic signs for the long-term success of anterior lamellar keratoplasty are the same as for penetrating keratoplasty, namely the presence of new vessels (neovascularization) in the corneal stroma, absence of corneal sensation, and severe dry eye.
Although the chances of rejection of anterior lamellar keratoplasty are lower than those of penetrating keratoplasty, the risk factors are the same as in penetrating keratoplasty, namely the presence of neovascularization, postoperative corneal infection / ulceration, and large-sized grafts.
Endothelial Keratoplasty
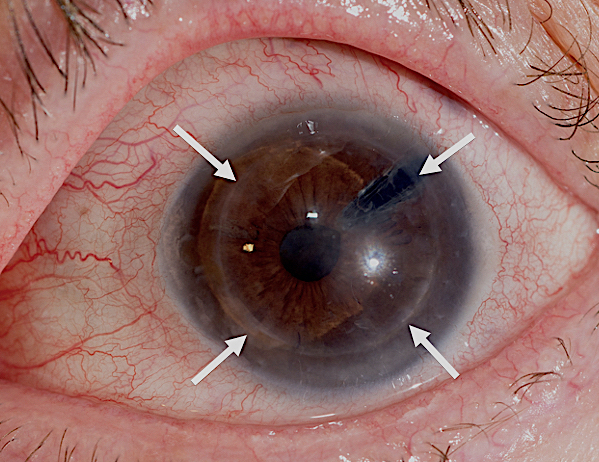
In some cases, it is only the inner layer of the cornea, the endothelium, that is damaged. Endothelial cells act as pumps that continuously remove water from the corneal stroma. Endothelial dysfunction leads to accumulation of water in the cornea, called corneal edema (swelling) and blurred vision. Endothelial keratoplasty aims to replace the diseased endothelium with healthy donor tissue.
The most common indications for endothelial transplantation are Fuchs endothelial dystrophy, bullous keratopathy (i.e. swelling / edema of the cornea after cataract or glaucoma surgery) and re-transplantation, when the first graft was either full-thickness or endothelial and has been rejected or malfunctions. Rarer indications include the iridocorneal endothelial syndrome (ICE syndrome) and the Axenfeld-Rieger syndrome.
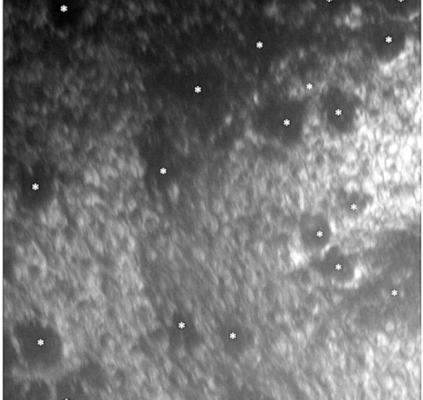
Fuchs Corneal Endothelial Dystrophy with Classic Guttae on Clinical Examination (white arrows) and Specular Microscopy (white asterisks)
There are two types of endothelial keratoplasty and the surgeon Dr. Palioura will discuss with you the type of transplant that is most suitable for you:
- DSAEK – Descemet Stripping Automated Endothelial Keratoplasty
- DMEK – Descemet Membrane Endothelial Keratoplasty
Both procedures aim to remove the dysfunctional endothelial cells and Descemet’s membrane through a small incision. The donor tissue is then inserted and positioned in their place and the incision is closed with 2-3 sutures. In both methods a large part of the cornea remains intact, so the risk of rejection of the new tissue is greatly reduced.
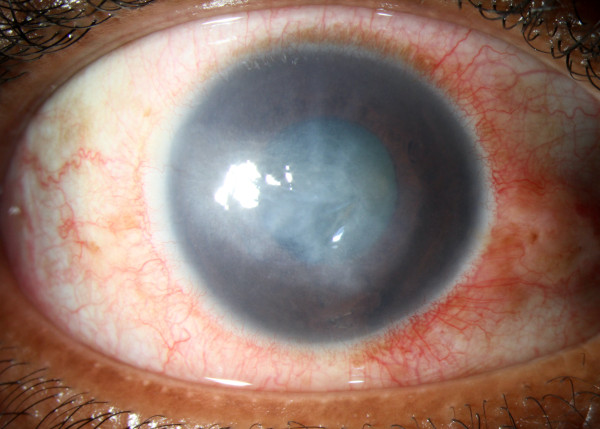
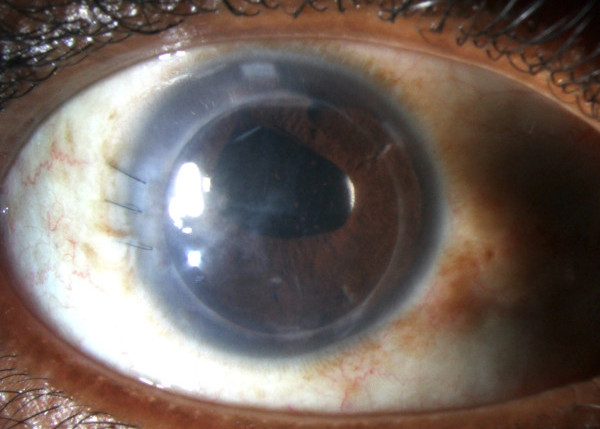
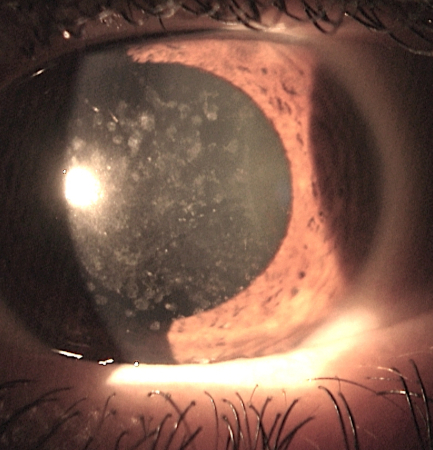
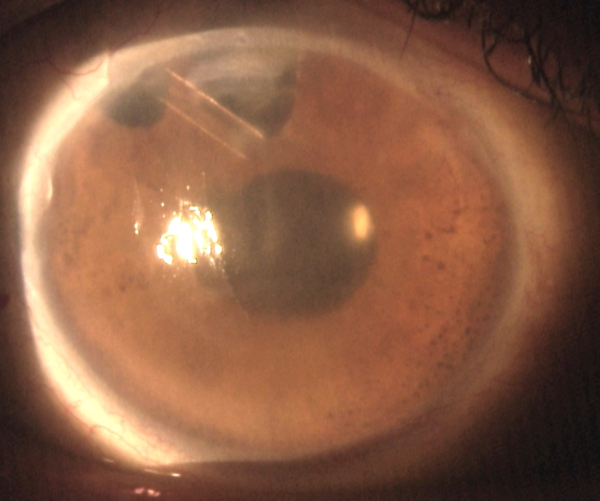
Significant Corneal Edema due to Iridocorneal Endothelial (ICE) Syndrome (left) Clear Cornea Two Months after Ultra-Thin Descemet Stripping Automated Endothelial Keratoplasty / DSAEK (right)
In DSAEK surgery, the donor tissue is thicker than the donor tissue used in DMEK surgery. This results in it being technically easier to manage and transplant. The surgeon Dr. Palioura uses the ultra-thin DSAEK technique using the EndoSerter device, which ensures the most atraumatic insertion of a very thin (thickness of 50 μm) donor tissue.
In DMEK surgery, the donor tissue is extremely thin and transplantation can be technically more difficult. Vision recovery, however, is faster because the tissue is thinner. Finally, the risk of graft detachment in the early postoperative period is greater compared to the DSAEK technique.
Before
After
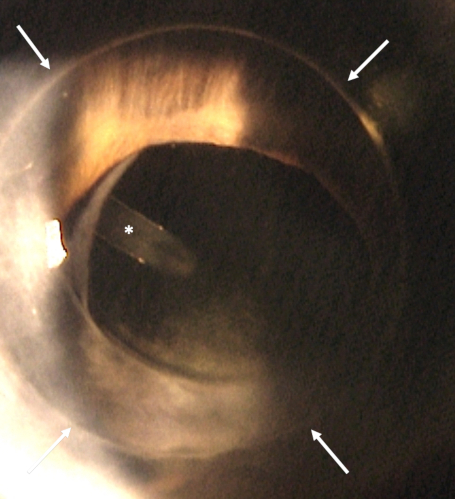
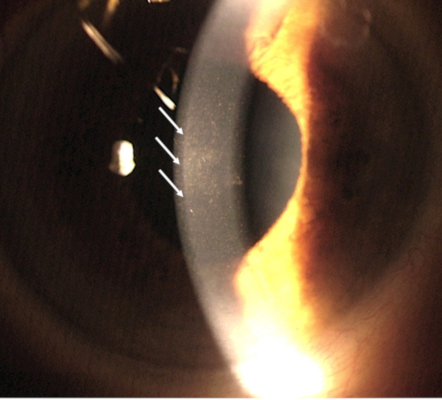
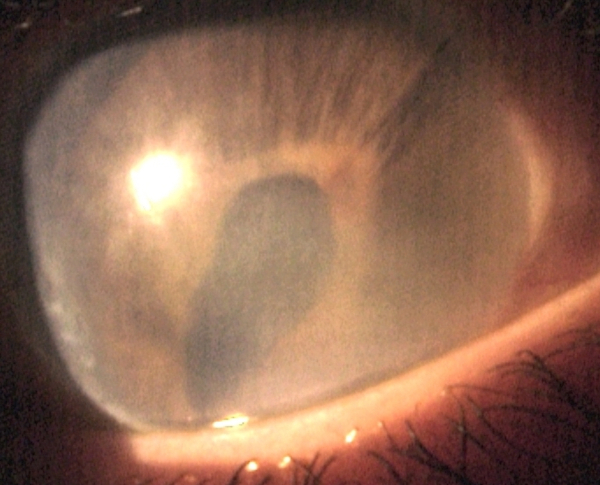
Chronic Corneal Edema and Ectopic Pupil due to Axenfeld-Rieger Syndrome and History of Glaucoma Tube and Six Months after Ultra-Τhin DSAEK (the white arrows show the edges of the corneal graft and the asterisk the tip of glaucoma tube)
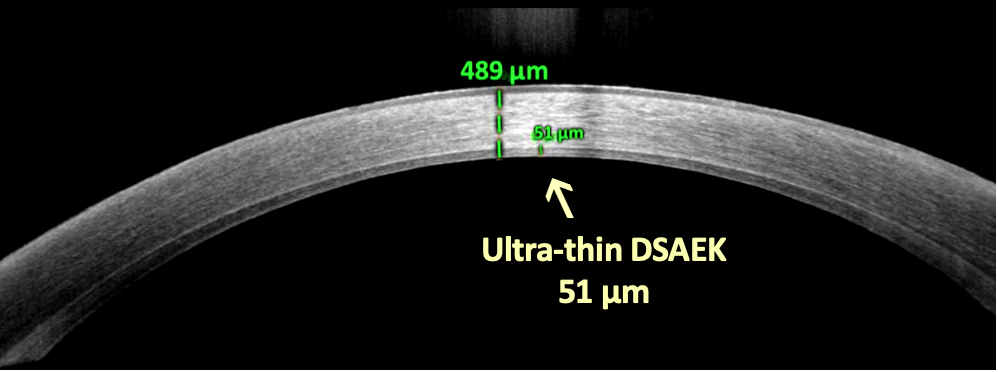
The Thickness of the Corneal Transplant is Only 51 μm on Anterior Segment Optical Coherence Tomography
In the early postoperative period, the most common complication is detachment of the endothelial graft from the patient's corneal stroma, which is treated by introducing additional air or gas into the anterior chamber to stabilize the graft. Subsequently, the most serious complication is infection at the interface between the graft and the patient's corneal stroma, which usually requires removal of the graft, intraocular antibiotic injections, and sometimes therapeutic full-thickness corneal transplantation.
Prognosis: In general, healing time after endothelial keratoplasty is shorter than after penetrating keratoplasty and anterior lamellar keratoplasty. Although the risk of endothelial graft rejection is lower compared to both penetrating keratoplasty and anterior lamellar keratoplasty, the risk factors for rejection are about the same as for penetrating keratoplasty and anterior lamellar keratoplasty, namely corneal neovascularization, postoperative corneal infection / ulceration, and graft-to-iris (iridocorneal) adhesions.
Before Corneal Transplantation Surgery
The surgeon Dr. Palioura will discuss with you the details of corneal transplantation surgery. She will discuss why you need this type of surgery, how it can help you see better, and what to expect during and after the surgery.
When you decide to proceed with corneal transplantation surgery, a possible date for the surgery will be set. This date may change if a good corneal donor tissue is not available on that day.
Chronic Corneal Edema / Pseudophakic Bullous Keratopathy After Cataract Surgery and Glaucoma Tube Shunt Surgery
It is important that you inform Dr. Palioura of all the medications you are currently on and she will confirm whether you can continue taking them before the surgery. You may need to stop using blood thinners before surgery. You may also need to see your family physician / GP or cardiologist for additional tests. This is to make sure you are healthy enough to undergo corneal transplantation surgery.
After the surgery, no hospitalization is required and you may return home. You will not be able to drive after corneal transplant surgery. You should arrange for a friend or relative to drive you home after the procedure.
On the Day of Corneal Transplantation Surgery
During your corneal transplant surgery, the following will take place:
- You will be given eye drops and possibly other medications by mouth to help you relax. Moreover, intravenous anesthesia will be used in combination with local anesthesia (monitored anesthesia care or MAC) or - more rarely - general anesthesia, so that you do not feel any pain or discomfort during the operation.
- Dr. Palioura will place a special device (eyelid speculum) in your eye to keep it open. Although your eye will be open, you will see little or nothing due to the anesthesia.
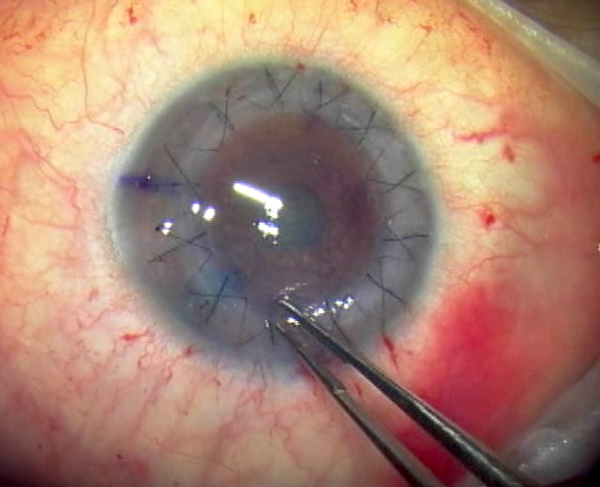
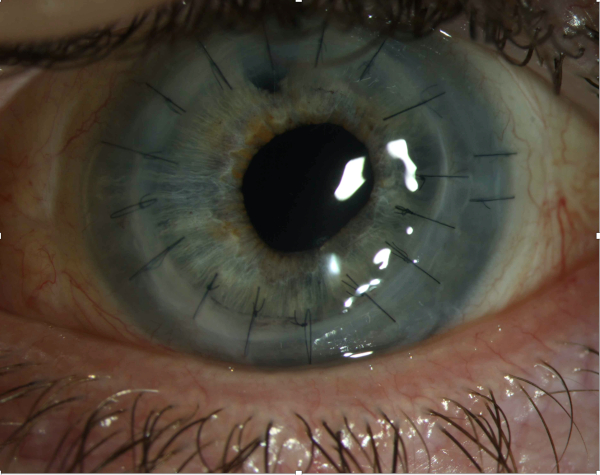
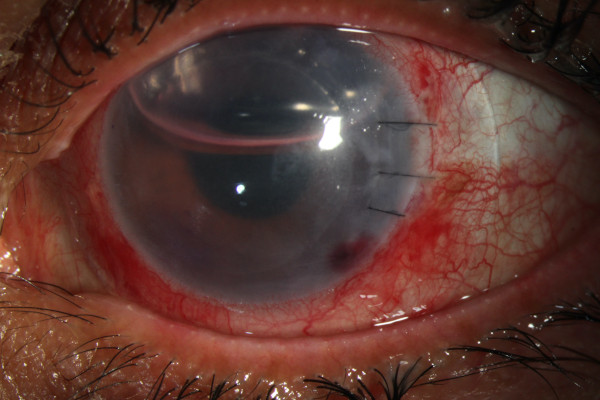
Intraoperative Photograph during Suture Adjustment at the end of Full-Thickness Corneal Transplantation (Penetrating Keratoplasty) in a Patient with Advanced Keratoconus
- Depending on the type of transplant you need, the surgeon will perform the necessary actions, such as:
- In penetrating keratoplasty, Dr. Palioura will remove a circular portion of your cornea and replace it by sewing in place a matching section of the donor cornea.
- In deep anterior lamellar keratoplasty (DALK), the surgeon Dr. Palioura will remove only the anterior part of the cornea, sewing the corresponding donor tissue in place.
- In endothelial keratoplasty, Dr. Palioura will remove only the dysfunctional inner layer of the cornea and replace it with a healthy donor tissue on the back surface of the cornea. She will then insert an air bubble which will push this new layer of endothelial cells into place.
Depending on the case, Dr. Palioura may treat other issues in your eyes during the same surgery, such as cataracts.
At the end of the surgery, the surgeon will place a protective cover over your eye. After recovery from anesthesia, you will be able to go home safely. Dr. Palioura will explain what you need to do to take care of your eye at home until she sees you again the next day.
After Corneal Transplantation Surgery
The day after your corneal transplant surgery, you will need to return to the office for your first post-operative exam.
Depending on the type of transplant, you may need to lie on your back for a few days after surgery. This helps the new donor tissue stay in place after endothelial transplantation. The stitches from the surgery will be removed gradually over the next few months depending on the type of transplant you have.
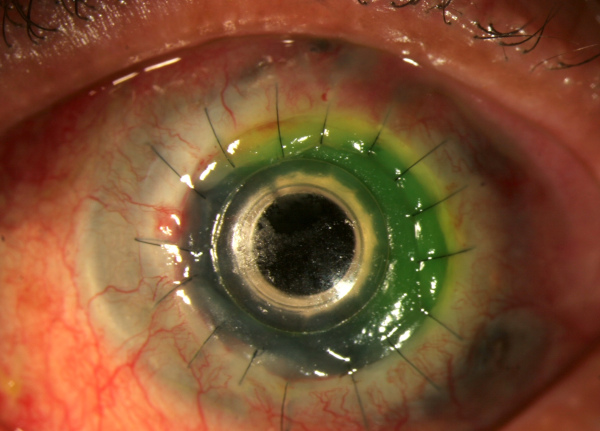
Air Bubble on Postoperative Day #1 After Ultra-Thin Descemet Stripping Automated Endothelial Transplantation in a Patient with Bullous Keratopathy
While recovering from corneal transplant surgery, you should be aware of the following:
- Use the eye drops exactly as prescribed by the ophthalmologist Dr. Palioura.
- Do not rub or push on your eyes.
- If you need a pain killer, ask the doctor which one you may take.
- Wear glasses or a protective cover to protect your eye.
- Discuss with the eye doctor when you can return to your normal daily routine.
Depending on the type of transplant and the healing rate of your eye, visual recovery can take anywhere from 1 month to 1 year.
Possible issues after a corneal transplant
Rejection of transplanted organs occurs when the body's immune system sees the transplanted tissue as something foreign and tries to get rid of it.
Warning symptoms of possible corneal graft rejection are:
- Eye pain
- Increased sensitivity to light (photophobia)
- Eye redness
- Blurred or cloudy vision
Inform your doctor immediately if you experience any of these symptoms so as to receive the right treatment that can stop and / or reverse the rejection episode. Rarely, a corneal transplant can cause other problems over time, such as infection or glaucoma (i.e. high eye pressure).
Even when the new corneal graft is working as it should, other eye problems can limit the quality of vision. For example, the new cornea may not have a smooth curvature; this is called astigmatism. Or you may already have or develop a retina problem such as macular degeneration, glaucoma or diabetic retinopathy, which also can limit your vision.
Third Postoperative Day after Boston Type 1 Keratoprosthesis Implantation in a Patient with History of Multiple Failed Corneal Grafts
Some patients need more than one corneal transplant, e.g. if the first transplant is rejected or becomes infected. However, a second transplant has a higher rejection rate than the first one did. After the third corneal transplant the chance of a fourth transplant being successful is very small. In such cases, the surgeon Dr. Palioura recommends implantation of a Type 1 Boston Keratoprosthesis, which is a form of artificial cornea.
Publications, Talks and Abstracts by Dr. Palioura on Corneal Transplantation
- Palioura, S., Chodosh, J., Pineda, R. (2012) A novel approach to the management of a progressive Descemet's membrane tear in a patient with keratoglobus and acute hydrops. Cornea 32:355-8.
- Palioura, S., Kim, B., Dohlman, C.H., Chodosh, J. (2013) The Boston keratoprosthesis type I in mucous membrane pemphigoid. The New England Ophthalmological Society (NEOS) Annual Meeting, Boston, MA, USA.
- Palioura, S., Kim, B., Dohlman, C.H., Chodosh, J. (2013) The Boston Keratoprosthesis type I in mucous membrane pemphigoid. Cornea 32:956-61.
- Palioura, S., Kim, B., Dohlman, C.H., Chodosh, J. (2013) The Boston keratoprosthesis type I in mucous membrane pemphigoid. Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting, Seattle WA, USA.
- Palioura, S., Chodosh, J. (2013) Keratoprosthesis. In Expert Techniques in Ophthalmic Surgery, eds. Spaeth, G., Ichhpujani, P., and Yanoff, M. JP Medical Publishers, London, UK.
- Palioura, S., Chodosh, J. (2013) Boston Keratoprosthesis Type II: indications, techniques, outcomes, and management. In Keratoprostheses and Artificial Corneas: Fundamentals and Surgical Applications, eds. Cortina, S., de la Cruz, J., Springer Science, Heidelberg, Germany.
- Palioura, S., Chodosh, J., Hart, L., Capaccioli, K., Ginat, D.T., Freitag, S.K. (2014) MRI, CT, and UBM imaging after corneal and cataract surgery. Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting, Orlando, FL, USA.
- Palioura, S., Colby, K. (2014) Outcomes of Descemet Stripping Endothelial Keratoplasty (DSEK) using Eye Bank-prepared pre-loaded grafts. American Academy of Ophthalmology (AAO) Annual Meeting, Chicago, IL, USA.
- Palioura, S., Ginat, D.T., Ashrafzadeh, A., Chodosh, J. (2014) Imaging after cornea surgery. In Post-treatment Imaging of the Orbit, eds. Ginat, D.T., Freitag, S., Springer Science, Heidelberg, Germany.
- Palioura, S., Colby, K. (2014) Outcomes of Descemet Stripping Endothelial Keratoplasty (DSEK) using Eye Bank-prepared pre-loaded grafts. The Aegean Cornea XII Meeting, Santorini, Greece.
- Palioura, S., Chodosh, J., Hart, L., Capaccioli, K., Ginat, D.T., Freitag, S.K. (2014) MRI, CT, and UBM imaging after corneal and cataract surgery. The New England Ophthalmological Society (NEOS) Annual Meeting, Boston, MA, USA.
- Palioura, S., Colby, K. (2015) Outcomes of Descemet Stripping Endothelial Keratoplasty (DSEK) using Eye Bank-prepared pre-loaded grafts. The 33th Annual Congress of European Society of Cataract and Refractive Surgery (ESCRS), Barcelona, Spain.
- Kontadakis, G., Palioura, S., Yoo, S. (2015) Wave-like interface opacities after Descemet stripping automated endothelial keratoplasty: 7 year follow-up. Eye and Contact Lens 43(4):e13-e15.
- Palioura, S., Colby, K. (2015) Outcomes of Descemet Stripping Endothelial Keratoplasty (DSEK) using Eye Bank-prepared pre-loaded grafts. Eye Bank Association of America Annual Meeting (EBAA), Atlanta, GA, USA.
- Palioura, S., Sivaraman, K.R., Sise, A., Batlle, J.F., Miller, D., Amescua, G., Karp, C.L. (2015) Fungal endophthalmitis after Descemet Stripping Automated Endothelilal Keratoplasty due to endogenously infected grafts from the same donor. The 49th Annual Meeting of the Ocular Microbiology and Immunology Group (OMIG), Las Vegas, NV, USA.
- Palioura, S., Colby, K. (2015) Outcomes of Descemet Stripping Endothelial Keratoplasty (DSEK) using Eye Bank-prepared pre-loaded grafts. World Cornea Congress, San Diego, CA, USA.
- Palioura, S., Kim, B., Dohlman, C.H., Chodosh, J. (2015) The Boston keratoprosthesis type I in mucous membrane pemphigoid. The 29th International Congress of the Hellenic Society of Intraocular Implant and Refractive Surgery, Athens, Greece.
- Palioura, S., Sivaraman, K.R., Sise, A., Batlle, J.F., Miller, D., Amescua, G., Karp, C.L. (2015) Fungal endophthalmitis after Descemet Stripping Automated Endothelilal Keratoplasty due to endogenously infected grafts from the same donor. The European Society of Cataract and Refractive Surgery (ESCRS) Winter Meeting, Athens, Greece.
- Palioura, S., Colby, K. (2015) Outcomes of Descemet Stripping Endothelial Keratoplasty (DSEK) using Eye Bank-prepared pre-loaded grafts. The 29th International Congress of the Hellenic Society of Intraocular Implant and Refractive Surgery, Athens, Greece.
- Παλιούρα, Σ. (2016) Κλινική Αξιολόγηση Μοσχευμάτων Κερατοειδούς με Σχισμοειδή Λυχνία. Σεμινάριο Εκπαίδευσης Ανάκτησης και Αξιολόγησης Μοσχευμάτων Κερατοειδούς, ΕΚΕΦΕ Δημόκριτος, Αθήνα.
- Palioura, S., Sivaraman, K.R., Sise, A., Batlle, J.F., Miller, D., Amescua, G., Karp, C.L. (2016) Fungal endophthalmitis after Descemet Stripping Automated Endothelilal Keratoplasty due to endogenously infected grafts from the same donor. The Aegean Cornea XIII Meeting, Chania, Greece.
- Gibbons, A., Palioura, S., Crane, A., Alfonso, E.C. (2016) Ramon Castroviejo does it again! The 34th Annual Congress of the European Society of Cataract and Refractive Surgery (ESCRS), Copenhagen, Denmark.
- Παλιούρα, Σ. (2016) Ο Ρόλος των Ομάδων Συγκομιδής στην Λειτουργία μιας Τράπεζας Οφθαλμών. Σεμινάριο Εκπαίδευσης Ανάκτησης και Αξιολόγησης Μοσχευμάτων Κερατοειδούς, ΕΚΕΦΕ Δημόκριτος, Αθήνα.
- Tsigkos, D., Tzelepi, A., Kopsini, D., Manolakou, D., Konistis, E. Palioura, S. (2017) Awareness and beliefs regarding cornea donation in Greece. The 35th Annual Congress of the European Society of Cataract and Refractive Surgery (ESCRS), Lisbon, Portugal.
- Palioura, S. (2017) Emergency Cornea Cases. The 31st International Congress of the Hellenic Society of Intraocular Implant and Refractive Surgery, Athens, Greece.
- Palioura, S., Colby, K. (2017) Outcomes of Descemet Stripping Endothelial Keratoplasty (DSEK) using Eye Bank-prepared pre-loaded grafts. Cornea 36(1):21-25.
- Tzelepi, A., Tsigkos, D., Kopsini, D., Manolakou, D., Konistis, E., Palioura, S. (2017) Awareness and beliefs regarding cornea donation in Greece. The 31st International Congress of the Hellenic Society of Intraocular Implant and Refractive Surgery, Athens, Greece.
- Tsigkos, D., Tzelepi, A., Kopsini, D., Manolakou, D., Konistis, E., Palioura, S. (2017) Awareness and beliefs regarding cornea donation in Greece. The 50th Annual Congress of the Hellenic Ophthalmological Society, Rhodes, Greece.
- Παλιούρα, Σ. (2017) Αρχές Λειτουργίας Τράπεζας Οφθαλμών και Κερατοειδούς. Πανεπιστημιακή Οφθαλμολογική Κλινική Νοσοκομείου Αθηνών «Γ. Γεννηματάς», Αθήνα.
- Palioura, S. (2017) Wet Lab Instruction Course: Procurement of Corneoscleral Rims for Residents. The 31st International Congress of the Hellenic Society of Intraocular Implant and Refractive Surgery, Athens, Greece.
- Palioura, S., Relhan, N., Leung, E., Chang, V., Yoo, S.H., Dubovy, S.R., MD, Flynn HW Jr. (2018) Delayed-onset Candida parapsilosis cornea tunnel infection and endophthalmitis after cataract surgery: histopathology and clinical course. American Journal of Ophthalmology Case Reports 11:109-114.
- Palioura, S. (2018) Cornea Imaging Beyond Tomography: Ultrasound Biomicroscopy, Optical Coherence Tomography and Confocal Microscopy. The 32nd International Congress of the Hellenic Society of Intraocular Implant and Refractive Surgery, Athens, Greece.
- Παλιούρα, Σ. (2018) Ετήσια Ανασκόπηση Κερατοειδούς 2018. Ετήσιο Συνέδριο Best of the American Academy of Ophthalmology 2018, Αθήνα.
- Palioura, S., Sivaraman, K., Joag, M., Sise, A., Batlle, J.F. Jr., Miller, D., Espana, E.M., Amescua, G., Yoo, S.H., Galor, A., Karp, C.L. (2018) Fungal endophthalmitis after Descemet Stripping Automated Endothelial Keratoplasty due to endogenously infected grafts from the same donor. Cornea 37(4):515-518.
- Palioura, S., Gibbons, A., Crane, A.M., Alfonso, E.C. (2018) Ramon Castroviejo does it again! Semi-autologous corneal transplantation with simultaneous bilateral surgery. The XIV Aegean Cornea Meeting, Mykonos, Greece.
- Παλιούρα, Σ. (2018) Ανασκόπηση Δημοσιεύσεων Κερατοειδούς και Οφθαλμικής Επιφάνειας 2018. Ετήσιο Οφθαλμόραμα της Ελληνικής Οφθαλμολογικής Εταιρείας, Αθήνα.
- Palioura, S., Relhan, N., Leung, E., Chang, V., Yoo, S.H., Dubovy, S.R., Flynn, H.W. Jr. (2019) Delayed-onset Candida parapsilosis cornea tunnel infection and endophthalmitis after cataract surgery: histopathology and clinical course. The 36th Annual Congress of the European Society of Cataract and Refractive Surgery, Paris, France.
- Παλιούρα, Σ. (2019) Κλινικές Ερωτήσεις στην Οφθαλμολογία. Ετήσιο Συνέδριο της Οφθαλμολογικής Εταιρείας Κεντρικής Ελλάδας, Λάρισα.
- Παλιούρα, Σ., Relhan, N., Leung, E., Chang, V., Yoo, S.H., Dubovy, S.R., Flynn, H.W. Jr. (2019) Χρόνια λοίμωξη κερατοειδικής τομής από Candida parapsilosis και ενδοφθαλμίτιδα μετά από χειρουργική επέμβαση καταρράκτη: ιστοπαθολογική έκθεση και κλινική πορεία. 52ο Πανελλήνιο Οφθαλμολογικό Συνέδριο, Αθήνα.
- Palioura, S., Vingopoulos, F., Likht, N., Piedra, C.M., Dubovy, S.R., Karp, C.L. (2019) Endothelial cell loss in cornea grafts from donors who sustained airbag injury or gunshot wound to the head. The 10th Annual EuCornea Congress, Paris, France.
- Palioura, S., Relhan, N., Leung, E., Chang, V., Yoo, S.H., Dubovy, S.R., Flynn, H.W. Jr. (2019) Delayed-onset Candida parapsilosis cornea tunnel infection and endophthalmitis after cataract surgery: histopathology and clinical course. The XVI Bi-annual Aegean Retina Meeting, Mykonos, Greece.
- Παλιούρα, Σ. (2019) Μεταμοσχεύσεις Κερατοειδούς. Πανεπιστημιακή Οφθαλμολογική Κλινική Αττικού Νοσοκομείου Αθηνών, Αθήνα.
- Palioura, S., Vingopoulos, F., Likht, N., Piedra, C.M., Dubovy, S.R., Karp, C.L. (2019) Endothelial cell loss in cornea grafts from donors who sustained airbag injury or gunshot wound to the head. The 36th Annual Congress of the European Society of Cataract and Refractive Surgery, Paris, France.
- Tsigkos, D., Tzelepi, A., Kopsini, D., Manolakou, D., Konistis, E., Palioura, S. (2020) Interactive online survey raises awareness about cornea donation. British Medical Journal Open Ophthalmology 4;5(1):e000285. doi: 10.1136/bmjophth-2019-000285.
- Palioura, S. (2020) Ultra-thin DSAEK using the EndoSerter insertion device in a patient with Axenfeld-Rieger syndrome and a pars plana glaucoma tube. The 34th International Congress of the Hellenic Society of Intraocular Implant and Refractive Surgery, Athens, Greece.
- Palioura, S. (2020) Ultra-thin DSAEK using the EndoSerter insertion device in a patient with Axenfeld-Rieger syndrome and a pars plana glaucoma tube. The 53rd Annual Congress of the Hellenic Ophthalmological Society, Thessaloniki, Greece.
- Palioura, S. (2020) Ultra-thin DSAEK using the EndoSerter insertion device in a patient with Axenfeld-Rieger syndrome and a pars plana glaucoma tube. The 38th Annual Congress of the European Society of Cataract and Refractive Surgery, Amsterdam, The Netherlands.
- Palioura, S., Tsiampali, C., Dubovy, S.R., Yoo, S.H. (2021) Endothelial biopsy for the diagnosis and management of culture-negative retrocorneal fungal keratitis with the assistance of OCT imaging. Cornea 40:1193-1196.
- Palioura, S., Vingopoulos, F., Likht, N., Piedra, C.M., Fout-Caraza, E., Dubovy, S.R., Karp, C.L. (2020) Endothelial cell loss in cornea grafts from donors who sustained gunshot wound to the head or airbag deployment in a motor vehicle accident. Cornea doi: 10.1097/ICO.0000000000002563.
- Palioura, S. (2022) Penetrating Keratoplasty Wetlab. The 36th International Congress of the Hellenic Society of Intraocular Implant and Refractive Surgery, Athens, Greece.
- Giachos, I., Angelidis, C.D., Doumazos, S., Tzavara, C., Palioura, S. (2022) Outcomes of combined penetrating keratoplasty and limbal stem cell transplantation: simultaneous versus sequential surgery. The 13th Annual EuCornea Congress, Athens, Greece.
- Tsigkos, D., Palioura, S., Theodorou, C., Gkogkou, K., Zouzoulas, E., Tsigkos, V. (2022) “Blast from the past: AKs to the rescue.” Manual arcuate astigmatic keratotomies for post-keratoplasty very high corneal astigmatism. The 13th Annual EuCornea Congress, Athens, Greece.
- Giachos, I., Angelidis, C.D., Doumazos, S., Tzavara, C., Palioura, S. (2022) Outcomes of combined penetrating keratoplasty and limbal stem cell transplantation: simultaneous versus sequential surgery. The 36th International Congress of the Hellenic Society of Intraocular Implant and Refractive Surgery, Athens, Greece.